As was reported in Socialist Voice in September 2020, the apparently systematic transfer of acute hospital patients to nursing homes, and the ensuing outbreaks and deaths, constitute a scandal of drastic proportions for the Irish state.
The facts surrounding this tragic situation require analysis, while official reports have been criticised for taking a conservative and uncritical approach to the role of the state and governmental decisions in creating or exacerbating it.
There is a common phrase about the transmission of covid-19 that we see repeated frequently by politicians and establishment figures, including the CEO of Nursing Homes Ireland,[1] the body that represents Ireland’s 400+ private nursing-homes: that “the prevalence of covid-19 within the community” has a knock-on effect of high levels of the virus within nursing-homes and other care settings.
While undeniably true to some extent, this really only tells half the story, given that we now know that some 2,300 hospital patients were transferred to nursing-homes between January and March last year,[2] on the pretext of freeing up general ICU capacity, resulting in outbreaks that have ultimately contributed almost half the total covid-related deaths in this country occurring in nursing-homes.[3]
There is community transmission—i.e. transmission that occurs as a result of the “normal” operation of everyday life, restrictions notwithstanding—and there is transmission as a result of decisions taken by the state, businesses and property-owners that create high-risk situations for the spread of the virus. Not surprisingly, it is only the former that we ever hear about, or that is subjected to scrutiny, particularly when the latter, being caused by exceptional, positive actions, are ostensibly more avoidable.
For example, alarmingly, the first term of reference for the Expert Panel tasked by the 26-County government with reporting on the response to covid-19 in nursing-homes was “to provide assurance that the national protective public health and other measures adopted to safeguard residents in nursing homes, in [the] light of COVID-19, are appropriate, comprehensive and in line with international guidelines . . .”[4]
Any sane person might expect an expert panel to be tasked with ascertaining whether the measures taken were appropriate, rather than providing assurance that they were. It is hard to imagine any other walk of life in which such a term of reference would be considered acceptable due diligence for a reporting body.
It is not until we get to the report’s recommendation 4.1, more than a hundred pages in, that some culpability on the part of the HSE is (indirectly) identified, when it urges that it should “ensure [that] all new residents coming from the community or proposed transfers from hospital are tested for COVID-19 prior to admission.” It is notable that HIQA’s own figures (see the graph) show a dramatic spike in reported deaths in nursing-homes that coincides with the mass inward transfer of hospital patients up to mid-March 2020 (week 13).[5]
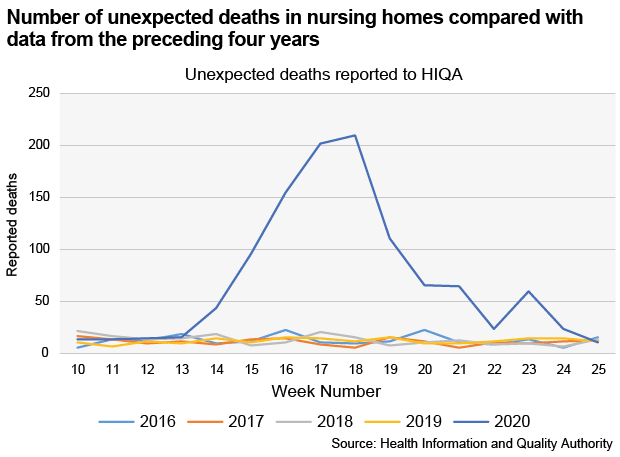
Ireland’s first case of the virus was reported on 29 February 2020, with new admissions to nursing-homes apparently continuing without mandatory testing up until June 2020, when the HSE’s guidelines were changed.[6] The increase in the “unexpected deaths” figure from week 13, as well as the generally accepted statistical lag of two to eight weeks from covid-19 cases to deaths,[7] suggest that it is possible for covid to have made its way into nursing-homes earlier than, or at least contemporaneous with, the first reported case in Ireland.
Both the report of the expert panel and HIQA have been criticised, by Age Action, among others,[8] for failing to adequately investigate the circumstances surrounding nursing-home deaths, or to provide an analysis of the level of care made available to those who died with covid-19 in nursing-homes in the past year.
We are compelled to add the following questions: Why were high-risk patients transferred en masse from acute hospitals to nursing-homes, some of which had covid-19 outbreaks, in the first few months of the pandemic? Who then bears responsibility for the resulting deaths, which were by any metric avoidable and therefore all the more tragic as a result?
By the HSE’s own figures there are 575 nursing-homes in the 26 Counties, comprising some 30,000 residents, of which 461 are private and voluntary nursing-homes. Covid-19 has now accounted for almost 2,000 deaths in these settings since the pandemic began—in other words over 6 per cent of the total number of residents. Comparatively, 4,610 people, or 0.096 per cent of the population of the state, have died from covid-19 at the time of writing (24 March 2021). Was this avoidable? Was it by design, or through human error?
If the latter, why no culpability still? Surveying the compliant national media, it is disturbing to note that “putting on the green jersey” extends to accepting, ignoring or defending (as appropriate) any and all malign decisions taken by the state in its response to covid-19.
A convenient narrative of personal responsibility über alles has been peddled by the state, big business, and the media, characteristic of their general policy of only telling us half the story, in order to absolve the ruling class and their allies of any culpability in this crisis. We reject this simplistic line of thinking, not because personal responsibility is unimportant—human solidarity means we must do what we can to protect one another in our own lives—but because as Marxists we attest that, just as we cannot shop our way out of the climate crisis through “greener” consumer choices, we cannot hand-wash our way out of the covid pandemic.
In fact all those efforts come to naught without commensurate responsibility being taken at all levels of society, but in particular by those who own the means of production, who co-ordinate legislation and travel, and who manage the complex but vital logistics of running a country. And if history has taught us one thing it is that those in power will not take action against their own interests unless they are made to by the force of the people.
References
- Age Action, Submission to the Oireachtas Special Committee on Covid-19 Response, September 2020 (https://www.oireachtas.ie/en/debates/debate/joint_committee_on_health/2021-02-02/2/).
- Paul Cullen, “Patient transfers into nursing homes may have been as high as 2,300,” Irish Times, 16 June 2020 (https://www.irishtimes.com/news/health/patient-transfers-into-nursing-homes-may-have-been-as-high-as-2-300-1.4280915).
- Midwest Radio, “43% of all deaths from covid-19 associated with nursing home outbreaks,” 12 March 2021 (https://www.midwestradio.ie/index.php/news/45970-43-of-all-deaths-from-covid-19-associated-with-nursing-home-outbreaks).
- Department of Health, “Covid-19 Nursing Homes Expert Panel: Final Report,” 19 August 2020 (https://www.gov.ie/en/publication/3af5a-covid-19-nursing-homes-expert-panel-final-report/).
- Health Information and Quality Authority, “The Impact of Covid-19 on Nursing Homes in Ireland,” July 2020 (https://www.hiqa.ie/sites/default/files/2020-07/The-impact-of-COVID-19-o n-nursing-homes-in-Ireland_0.pdf).
- Paul Cullen, “New care home residents must be tested for covid-19 under rule change,” Irish Times, 3 June 2020 (https://www.irishtimes.com/news/health/new-care-home-residents-must-be-tested-for-covid-19-under-rule-change-1.4269793).
- Harvard University School of Public Health, “Data animation shows time lag between covid-19 cases and deaths” (https://www.hsph.harvard.edu/news/hsph-in-the-news/data-animation-shows-time-lag-between-covid-19-cases-and-deaths/).
- Age Action, Submission to the Oireachtas Special Committee on Covid-19 Response, September 2020 (https://www.oireachtas.ie/en/debates/debate/joint_committee_on_health/2021-02-02/2/).